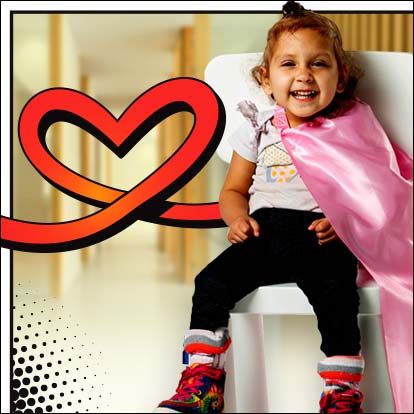
Help Unlock a Child’s Superpowers!
Make a gift and a kid like Naomi will get the book "What Makes a Superhero?"
Give Today
Pediatric Specialty Care in Northern California

The Shriners Children's Northern California Neil Reitman Pediatric Burn Institute provides care with distinction to children.
About Shriners Children's Northern California
Minutes from downtown Sacramento, our experienced, compassionate team brings hope and healing. We're driven to make lives richer, easier and less complex for children and their families throughout Northern California, the Western U.S., Northwestern Mexico and Canada.
Specialty Care Provided in Northern California
We Understand the Unique Medical Needs of Children
We provide vital, pioneering treatment from birth to age 18. Here, children have the opportunity to be evaluated and treated by doctors recognized as the best by their peers.





What's Happening at Shriners Children's Northern California
-
Bracing Against the Curve: Anakalia’s Story of Strength and Support from Shriners Children’s
-
Shriners Children’s Northern California Heals Dan in Many Ways
-
Shriners Children’s Northern California Hosts 33rd Annual Ashley Lectureship Series
-
Inpatient Rehabilitation Program is a Bridge to Life After Traumatic Injuries
UPCOMING EVENTS
Help Us Provide the Gift of Hope and Healing
Every gift has an impact, which is why there are multiple ways you can help.
Keep In Touch
Join our mailing list to stay up to date on everything that's happening at Shriners Children's.










